Do you struggle with
freezing of gait?
Do you struggle with
freezing of gait?
Would you like to take part in a study of a new investigational treatment for freezing of gait?
We’re inviting people with Parkinson’s to take part in a clinical research study to evaluate CereGate Therapy for freezing of gait.

Would you like to take part in a study of a new investigational treatment for freezing of gait?
We’re inviting people with Parkinson’s to take part in a clinical research study to evaluate CereGate Therapy for freezing of gait.

Research moves us forward
CereGate Therapy
CereGate Therapy involves adding an additional program to your existing DBS system for you to use while walking. This program is intended to create rhythmic sensation to prompt, or “cue” you to step while walking. The aim is to explore whether this could function as an internal cue—similar to external cues like a metronome—to determine whether it helps reduce freezing of gait.
Research moves us forward
CereGate Therapy
CereGate Therapy involves adding an additional program to your existing DBS system for you to use while walking. This program is intended to create rhythmic sensation to prompt, or “cue” you to step while walking. The aim is to explore whether this could function as an internal cue—similar to external cues like a metronome—to determine whether it helps reduce freezing of gait.
What’s involved
(at a glance)
What’s involved
(at a glance)
“Our technology offers the possibility of helping people with Parkinson’s maintain their independence a little longer. Your participation in this study helps us answer important questions such as: does it work, and how effective is it?“
Brian Blischak
President CereGate Inc.
“Our technology offers the possibility of helping people with Parkinson’s maintain their independence a little longer. Your participation in this study helps us answer important questions such as: does it work, and how effective is it?”
Brian Blischak
President CereGate Inc.
If everyday steps matter to you, consider taking the next step with us.
No one understands the challenge of freezing of gait better than you do. That’s exactly why your contribution to this research is so important. Your participation in our study could make a real difference in improving treatment for many people living with Parkinson’s.
If everyday steps matter to you, consider taking the next step with us.
No one understands the challenge of freezing of gait better than you do. That’s exactly why your contribution to this research is so important. Your participation in our study could make a real difference in improving treatment for many people living with Parkinson’s.
How Does the Study Work?
A Look Behind the Scenes
We understand that joining a clinical study can bring up a lot of questions. That’s why we want to walk you through every step—openly and clearly. You might be surprised by how simple and straightforward it really is.
The Scientific Idea: A Rhythm from Within
How Does the Study Work?
A Look Behind the Scenes
We understand that joining a clinical study can bring up a lot of questions. That’s why we want to walk you through every step—openly and clearly. You might be surprised by how simple and straightforward it really is.
The Scientific Idea: A Rhythm from Within
What you can expect
What you can expect

Phase 1
Screening (2 Visits)
• Informed Consent:
The study team will give you an informed consent document that explains the study’s purpose, procedures, potential risks and benefits, and your rights. They will review the document with you, answer all your questions, and ask you to sign the document.
• Eligibility Check and Baseline Data:
The study team will ask you some questions, and ask you to perform some tasks to evaluate your Parkinson’s and freezing. The purpose is to confirm that you meet all the criteria to join the study, and to collect baseline data. You will abstain from taking your Parkinson’s medications the morning of the second visit.

Phase 1
Screening (2 Visits)
• Informed Consent:
The study team will give you an informed consent document that explains the study’s purpose, procedures, potential risks and benefits, and your rights. They will review the document with you, answer all your questions, and ask you to sign the document.
• Eligibility Check and Baseline Data:
The study team will ask you some questions, and ask you to perform some tasks to evaluate your Parkinson’s and freezing. The purpose is to confirm that you meet all the criteria to join the study, and to collect baseline data. You will abstain from taking your Parkinson’s medications the morning of the second visit.

Phase 2
Starting CereGate Therapy
• More Baseline Data:
Similar to the second study visit, you will be asked some questions, and asked to perform some tasks to evaluate your Parkinson’s and freezing.
• Starting CereGate Therapy:
Your DBS system will be reprogrammed to add an extra program. You will be taught how and when to use the extra program.

Phase 2
Starting CereGate Therapy
• More Baseline Data:
Similar to the second study visit, you will be asked some questions, and asked to perform some tasks to evaluate your Parkinson’s and freezing.
• Starting CereGate Therapy:
Your DBS system will be reprogrammed to add an extra program. You will be taught how and when to use the extra program.

Phase 3
At-Home Use (Approximately 60 days)
• Real-world Use:
You will use CereGate therapy as-needed in your daily activities. One day each week you will complete a diary to document any freezing or falls that occurred on that day.
• On-going support:
Every two weeks you’ll have a 15-20 minute phone call with the study team. You’ll also have a phone number that you can use to call them 24/7 if you have any problems.

Phase 3
At-Home Use (Approximately 60 days)
• Real-world Use:
You will use CereGate therapy as-needed in your daily activities. One day each week you will complete a diary to document any freezing or falls that occurred on that day.
• On-going support:
Every two weeks you’ll have a 15-20 minute phone call with the study team. You’ll also have a phone number that you can use to call them 24/7 if you have any problems.

Phase 4
Final Assessment (2 Visits)
• Wrap up visits:
The study team will complete the data collection by asking you the same types of questions asked in the first 3 visits (plus a few more), and asking you to perform the same tasks to evaluate your Parkinson’s and freezing.

Phase 4
Final Assessment (2 Visits)
• Wrap up visits:
The study team will complete the data collection by asking you the same types of questions asked in the first 3 visits (plus a few more), and asking you to perform the same tasks to evaluate your Parkinson’s and freezing.
How do we measure progress?
How do we measure progress?
Freezing of gait often appears suddenly and unpredictably—making it hard to measure. That’s why we combine your personal feedback with clinical observations and electronic measurements.
Freezing of gait often appears suddenly and unpredictably—making it hard to measure. That’s why we combine your personal feedback with clinical observations.
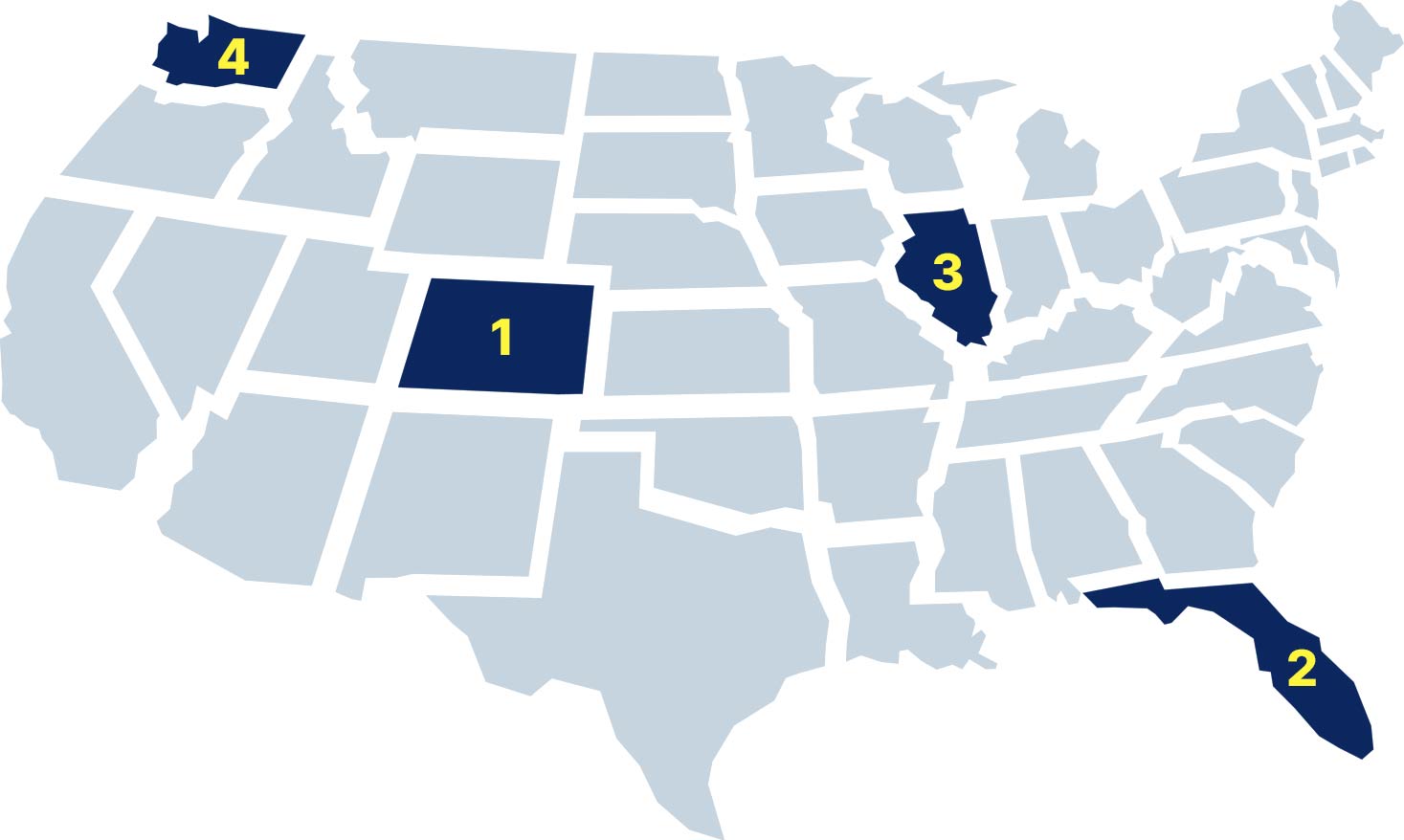
Find a Study Center Near You:
This study is being conducted at carefully selected, leading clinics across the U.S.
We understand that travel can be a challenge—for you and your loved ones. Use the map to see if there’s a location within reach. Even if distance feels like a concern, we encourage you to complete the eligibility questionnaire. There may be support options available to help with travel.
Find a Study Center Near You:
This study is being conducted at carefully selected, leading clinics across the U.S.
We understand that travel can be a challenge—for you and your loved ones. Use the map to see if there’s a location within reach. Even if distance feels like a concern, we encourage you to complete the eligibility questionnaire. There may be support options available to help with travel.
For Care Partners and Loved Ones

We know your role goes far beyond just providing support. You are often the steady hand, the most trusted advisor, and the driving force when it comes to exploring new options. Your confidence and trust are essential to us, and we want to answer your most important questions directly.
For Care Partners and Loved Ones

We know your role goes far beyond just providing support. You are often the steady hand, the most trusted advisor, and the driving force when it comes to exploring new options. Your confidence and trust are essential to us, and we want to answer your most important questions directly.
Frequently Asked Questions
Frequently Asked Questions
About the Study and the Therapy
About the Study and the Therapy
Participation and Eligibility
Participation and Eligibility
Process and Commitment
Process and Commitment
Costs, Risks, and Other Information
Costs, Risks, and Other Information
Let’s go
If you think you might like to participate in this freezing of gait study or would like more information, complete the survey below. If it looks like you may qualify, then you will be given the opportunity to immediately speak with a study representative (24/7), or to call them back at a more convenient time (24/7).
Let’s go
If you think you might like to participate in this freezing of gait study or would like more information, complete the survey below. If it looks like you may qualify, then you will be given the opportunity to immediately speak with a study representative (24/7), or to call them back at a more convenient time (24/7).